At Pulse Clinic, we are dedicated to providing comprehensive healthcare services that meet the diverse needs of our patients. With a team of highly skilled professionals and cutting-edge technology, we offer a wide range of medical services and diagnostic facilities to ensure your well-being. Here's an overview of the services we provide:
At Pulse Clinic, we are dedicated to providing comprehensive healthcare services that meet the diverse needs of our patients. With a team of highly skilled professionals and cutting-edge technology, we offer a wide range of medical services and diagnostic facilities to ensure your well-being. Here's an overview of the services we provide:
PULSE BREAST CLINIC
provides the region’s
most advanced breast care for women
including routine exams, screening and diagnostic mammograms for the detection of breast cancer, and education about general breast care.
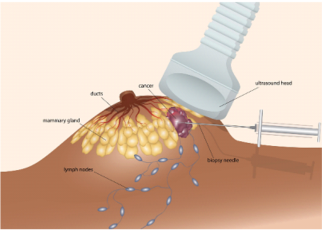
The clinical examination ,breast ultrasound ,mammogram and biopsies are all done in the single visit as far as possible.
Diagnostic facilities offered with state of the art technology and the very best in the world.
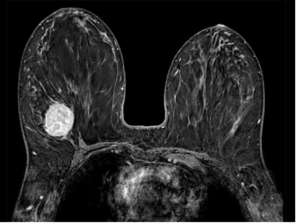
We brought in
3D mammography with tomosynthesis
in the year 2017 into Palakkad town ,
the first in a private diagnostic clinic in Kerala.